White Paper: The Future of Data Analytics and the Opioid Epidemic
White Paper: The Future of Data Analytics and the Opioid Epidemic
In 2020 Covid-19 and the opioid epidemic collided, creating a “twindemic” that overwhelmed healthcare providers, community organizations, and state and local governments.
While widespread vaccine distribution will mitigate Covid-19, the opioid epidemic endures – and evolves. Those suffering from opioid use disorder (OUD) are more at risk for relapse during times of stress, and disruptions in care and increased isolation likely contribute to an increase in opioid-related deaths in more than 40 states.
Fortunately, a number of state and local governments leveraged the data sharing and analytics programs already in place to combat substance use disorder and applied it to their pandemic responses. Now it’s time for state and local leaders to build on that progress and use the learnings of the past year to prepare for what’s next. With the American Rescue Plan and a surge of other opioid-related funding, state and local leaders must seize the opportunity to develop the data sharing programs and analytics tools they need to create innovative and data-driven solutions for addressing opioid abuse in their communities.
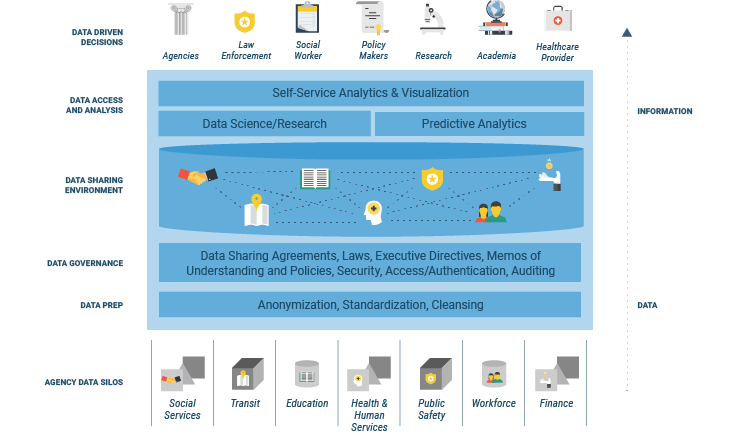
Building a High-Impact Substance Use Disorder Analytics Framework
Creating a statewide approach to substance use disorder begins with data sharing. Best-in-class frameworks will combine previously siloed data from different agencies, secretariats, localities, social services, public safety and corrections, drug courts, community coalitions and private healthcare systems. Through this framework, states can grasp insights critical to prevention, early intervention, treatment, and recovery.
Once the data sharing infrastructure and agreements are in place, business intelligence and analytics capabilities are layered in to turn the collective data into actionable insights.
Empowering Front Line Responders with Data Analytics
An effective data sharing program not only brings together data from the myriad of state and local agencies, but also gets that data into the hands of people on the front lines: EMS workers, local law enforcement, community treatment centers, etc. While some states have programs in place to measure the impact of the opioid crisis, next generation solutions must empower on-the-ground decision-making by community responders.
One way to funnel the right information to the local responders is incorporating a self-service analytics layer into the cross-agency data sharing program. This gives approved community organizations, both inside and outside the government, dashboards, reports, and data visualization tools they need to interpret data as they respond to the crisis. It’s important that the user experience is designed for non-technical users, not data scientists.
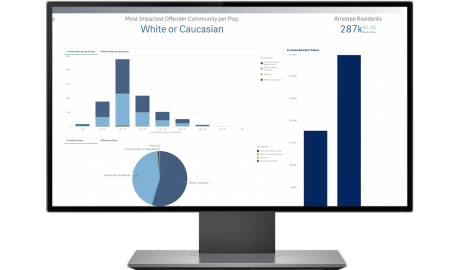 The best people to respond to the opioid epidemic are those who are on the front lines witnessing the effects of drug abuse within their own communities. A self- service analytics layer was designed to give community organizations powerful new tools to create reports and dashboards in a timely manner, view incident maps and more effectively collaborate as they respond to the crisis.
The best people to respond to the opioid epidemic are those who are on the front lines witnessing the effects of drug abuse within their own communities. A self- service analytics layer was designed to give community organizations powerful new tools to create reports and dashboards in a timely manner, view incident maps and more effectively collaborate as they respond to the crisis.
Once local responders have access to this powerful data, they can use it identify individuals who need help now, as well as those who may be more susceptible to opioid use in the future based on their individual circumstances.
Potential insights include,
- Improve community education and social services outreach by understanding “Age of First Use” and “Age of First Arrest”
- Create early warning systems to predict regional overdose spikes and proactively distribute life-saving drugs to local responders
- Micro-target specific neighborhoods and streets that need intervention
- Adjust staffing of peer recovery specialists in hospitals and treatment centers
- Understand which Child Protective Services cases involve parental OUD and measure the outcomes of different intervention methods
Data Analytics and Preparing for Future Disruptions in Care
One of the reasons behind the spike in opioid overdoses during Covid was the sudden drop in availability of healthcare services. While we can’t predict when we’ll experience an event as disruptive as the pandemic again, state and local leaders can use data analytics to mitigate the risk of future disruptions.
For example, by analyzing broadband internet access in comparison to substance use by region, local governments can identify neighborhoods that are unlikely to be able to access telehealth services, should stay-at-home orders be reinstated in the future. Healthcare providers could study the efficacy of telehealth treatment versus in-person treatment across age groups or other demographics to inform future programs.
Analytics can be used to gather a variety of insights related to future disruptions in care
- Study the outcomes of regulatory changes made during Covid-19 related to continuity of care, including the teleprescribing of buprenorphine, used to combat narcotic addiction
- Analyze waiting room capacity and hospital bed inventory across regions to identify areas at high risk of overcrowding if social distancing is required
- Identify overlaps in community services used by those with OUD to investigate opportunities to reach patients outside of traditional healthcare centers
Mitigating and Treating the Use of Multiple Substances
The number of overdoses involving multiple substances was on the rise well before 2020. In 2018, roughly 63% of opioid overdose deaths in the United States also involved cocaine, methamphetamine, or benzodiazepines, and deaths from overdoses involving synthetic opioids like Fentanyl were up 52% year-over-year in August of 2020.
Because of the rise in overdose deaths, experts recommend that efforts to reduce opioid overdoses should also include methods of mitigating the use of multiple substances. To do so, state and local government and community organizations must understand the prevalence of specific substances in their communities and the outcomes of those substances on the health of their constituents:
- Identify emerging trends in substance use by combining law enforcement data and hospital data
- Perform targeted analyses on fatal opioid overdoses involving multiple substances
- Improve law enforcement intervention programs by drilling down into details about arrests, including substances involved, time of arrest, location, and activity (e.g. buying/receiving)
 Combining Predictive Analytics and Social Determinants of Health
Combining Predictive Analytics and Social Determinants of Health
Predictive analytics has played a multifaceted role in the public sector’s response to substance use, from developing risk profiles to identifying physicians with the propensity to overprescribe pain killers. However, applying predictive analytics to isolated datasets without considering outside factors can be misleading.
Individuals who struggle in any of the five areas deemed “social determinants of health”—economic stability, education access and quality, social community and context, healthcare access and quality, and neighborhood and built environment— are more likely to experience poverty driven inequities in care and opioid addiction.
This is why data sharing is so important in developing a holistic community approach to substance use disorder. By integrating data from multiple sources, front line responders can have a clearer picture of the social and economic circumstances that are at play in their patients’ lives.
Consider the importance of SDOH context for treating patients with methadone or buprenorphine. The patient’s housing situation, access to transportation, and social community (e.g. whether or not the patient lives with others who use opioids) could have a dramatic effect on the efficacy of the treatment. By understanding these outside factors, treatment could be tailored to ensure the patient has continuous, uninterrupted access to medication.
Getting Started with a Data Analytics Framework
While the prospect of launching a statewide daring sharing initiative can seem overwhelming, state and local leaders can accelerate progress by embracing an agile approach and using proven data governance methods to secure buy-in from key stakeholders.

