How States Can Save Lives by Tracking and Sharing Data about Polysubstance Overdoses
How States Can Save Lives by Tracking and Sharing Data about Polysubstance Overdoses
The Biden-Harris administration recently designated fentanyl combined with xylazine, a tranquilizer typically used in veterinary medicine, as an “emerging threat” to the United States.
While this is the first time that a combination of illicit drugs has been labeled an “emerging threat” by a presidential administration, fatal overdoses involving multiple substances have been on the rise in communities across the United States for several years, according to the CDC. That’s one reason why efforts to reduce opioid overdoses must also include methods of tracking the use of emerging substances or common additives. Otherwise, by the time a drug is on the radar of the general public, many lives have already been lost.
But spotting shifts in usage or a surge in overdoses related to laced drugs can be difficult. When a drug contains many different substances, and the ratio of those substances varies by region—as is almost always the case—a substance may look relatively uncommon at the state level. Only when we drill down into the regional level can we see the actual trends.
Recognizing local usage patterns is the first step in preventing them from becoming statewide issues. Community organizations must understand the prevalence of specific substances in their communities and the outcomes of those substances on the health of their constituents.
By leveraging data and analytics, communities in Virginia are doing just that. Virginia’s Framework for Addiction Analysis and Community Transformation, developed in partnership with Voyatek, provides a secure, centralized data sharing hub for organizations across the Commonwealth, allowing coalitions and groups to have access to analytics tailored to their communities.
The ability to analyze both statewide and local trends has been a critical part of community efforts to stay ahead of emerging substances and dangerous additives. By partnering with Virginia’s Department of Forensic Science (DFS), FAACT analyzes lab cases by substance and location to pinpoint disproportionately impacted areas. In January 2022, for example, several counties began to see a spike in overdoses and criminal incidents involving xylazine.
Though the surge in xylazine usage was alarming for these communities, at the state level, xylazine usage during this time appeared relatively uncommon, peaking at 2.5% of substances tested by DFS statewide, as we see in this graph:
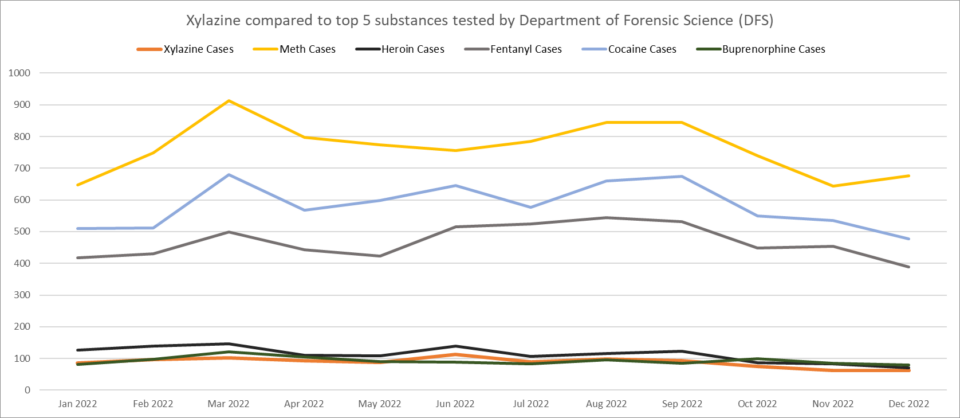
However, when analysts drilled down into the prevalence of xylazine by jurisdiction, it was clear that several communities were seeing dangerous amounts of xylazine circulating in the community. In Warren County, for example, xylazine accounted for 14% of DFS cases.
A year-over-year analysis of xylazine cases by jurisdiction confirmed that usage of the drug would likely spread from “hot spots” to surrounding counties:
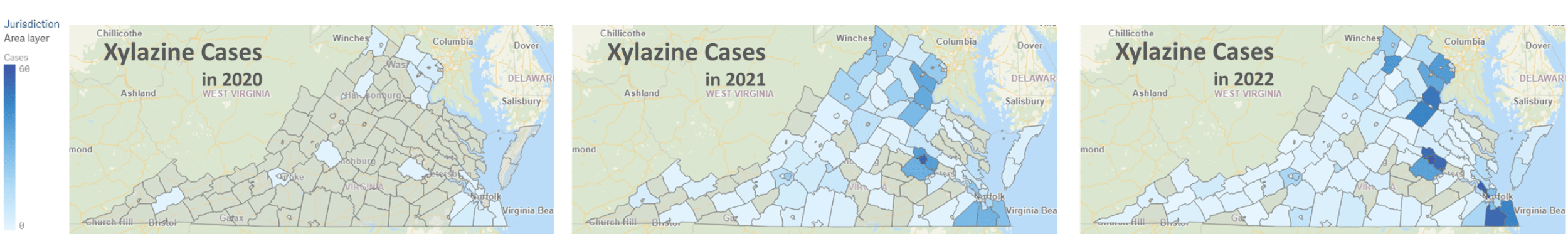
Fortunately, our analyst team identified these hot spots and worked with local opioid coalitions to get a head start on addressing xylazine usage, months before the CDC and FDA issued national alerts.
While xylazine is still present in Virginia, the early intervention slowed the surge in cases and played a role in preventing xylazine from becoming highly prevalent across the state.

